Tireoide e o consumo de proteína – a questão do “T3 e T4 livres”
A questão do artefato de laboratório chamado “hormônio livre” e a realidade dos carreadores proteicos
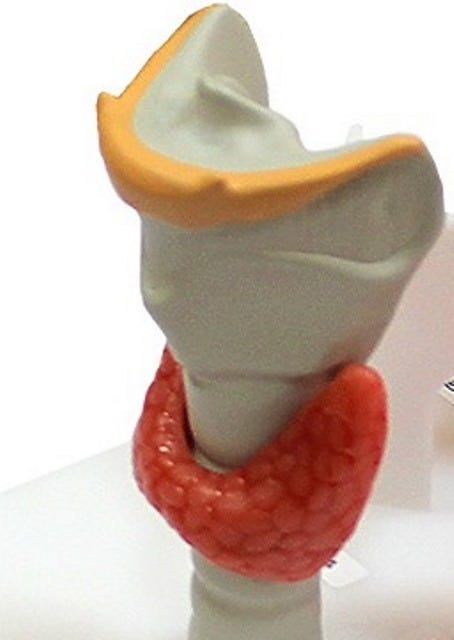
[Imagem: zamitza.ru]
Já foi explicado mais de uma vez que, se não forem oferecidos ao nosso organismo todos os nutrientes essenciais de que necessita – dentre eles uma dada quantidade de proteínas de qualidade todos os dias – ele entrará em estresse, em sofrimento,
E será desencadeada alguma estratégia biológica defensiva ou resposta adaptativa na linguagem de Hans Selye.
Dentro desse marco, esta nota escolheu focar a questão de como é carreado o hormônio tireoidiano, ativo e inativo, no nosso sangue, e como ele alcança os órgãos alvo. O sentido da nota é o de situar um pouco a questão crítica da demanda proteica alimentar.
Lembrando que o hormônio ativo somente terá efeito se entrar na célula e, ato contínuo, chegar lá na mitocôndria, onde ele, o T3, aciona a enzima chave da respiração celular oxidativa.
Amparando assim a produção da energia corporal.
Ora, a medicina dominante, por razões que não cabe focar aqui, está permeada de clichês e de mitos, inclusive em relação à tireoide.
Um dos clichês da medicina oficial é o de que existiria o hormônio tireoidiano “livre”, que esse hormônio “livre” é o que conta e que é assim, na condição de molécula livre, solta, que ele alcança a célula, entra no citoplasma, mitocôndria e núcleo, para exercer seu efeito.
Várias experiências, no entanto, mostram o contrário do clichê. E que o hormônio tireoidiano – quaisquer dos dois, ativo e inativo – necessita ser carreado por outras moléculas, especialmente proteínas.
Mostram, por exemplo, que o hormônio penetra na mitocôndria depois de ser carreado por proteínas ou lipoproteínas ao longo do trajeto que separa o fígado [onde é ativado, ou da própria tireoide] em direção à membrana mitocondrial.
Portanto o hormônio tireoidiano [T4, T3] precisa de ser transportado, ele não viaja e nem penetra na célula solto, free.
A doutrina do hormônio tireoidiano “livre” pode ser facilmente dispensada a partir das evidências, arroladas por R. Peat em artigo já antigo [Thyroid therapies, confusion and fraud], onde ele mostra que o T3 é carreado no plasma associado a três tipos de mediadores, a proteínas [pré-albumina ou transtirretina; albumina, globulina tipo TBG], também a gorduras do tipo lipoproteínas [HDL, LDL, VLDL] e, por último, às hemácias [S][T].
Na verdade, quase todo o T3 é carreado no plasma pelas hemácias, isto é, 95% dele. Ou seja, a concentração de T3 na hemácia é de 15 a 50 vezes maior do que nas proteínas do plasma.
E é por isso mesmo que medir o T3 como é usualmente feito pelos laboratórios, medir no plasma, descartando as hemácias, é uma medida de valor duvidoso.
Na verdade, esse procedimento joga fora quase todo o T3 que se pensa estar medindo. Tudo isso em nome de achar o tal “hormônio livre”. Fica parecido com outro clichê da medicina dominante, de ver no colesterol, fantasmagoricamente, a molécula que ele não é e ficar imaginando que é inflamatório quando é exatamente o contrário, uma das moléculas mais protetoras do nosso organismo.
No caso do “hormônio livre” estamos diante de uma fantasmagoria dispensável para explicar seu transporte, maciçamente feito, como foi dito instalado nas hemácias. A doutrina do “T3 livre” tem pouco a explicar quanto ao seu transporte. As hemácias são seu principal transportador, e por um mecanismo de pura afinidade eletrônica, sem gasto de energia. Da hemácia o T3 se liga à proteína que entra no citoplasma por difusão e dali chega ao seu principal alvo fisiológico, a enzima respiratória.
T3 é captado e acumulado nas hemácias através de um sistema carreador especifico mediado” [H].
O hormônio ativo, portanto, é aquele ligado a proteína, protein-bound.
É dessa forma que o T3 viaja [C], que penetra no cérebro, onde, aliás, ele se concentra seis vezes mais que no plasma [D][E].
“Se o T3 ligado ao conjunto da célula pode exercer sua ação hormonal, por que deveríamos pensar no hormônio ligado a proteína como sendo incapaz de afetar as células? A ideia de medir o ´hormônio livre´ que supostamente representaria o hormônio biologicamente ativo, deveria dar lugar à avaliação, mais fácil, dos efeitos biológicos do hormônio do que medir aquela entidade hipotética”[R. Peat].
E já se descobriu que “o T3 encontra-se fortemente associado com as proteínas citoplasmáticas da célula, ao mesmo tempo em que se move rapidamente entre elas e em relação a outras proteínas de fora da célula”[R. Peat]. Sempre associado a elas.
Em nenhum momento se torna necessário aquele clichê para explicar os movimentos do T3. O que torna, em consequência, o exame laboratorial do hormônio “livre” [seja T3 ou T4] pouco mais que inútil.
Ou, na imagem de R. Peat, se o botão consegue fechar a blusa, por que alguém precisaria recorrer a à imagem de cinco anjos segurando o botão ou qualquer “explicação” no estilo? O transporte do hormônio tireoidiano já tem explicação suficiente para poder dispensar a hipótese do hormônio “livre”. E no entanto, os doutores e seus laboratórios continuam medindo o “hormônio livre”.
Também no caso da entrada das proteínas carreadoras do T3 para dentro da célula: por que buscar explicações do tipo endocitose - o que levaria a gasto de energia – quando tudo pode ser explicado por difusão? Por exemplo, já se sabe que o T3 é carreado pela albumina, atraído por cargas elétricas opostas da proteína, operando como T3-albumina e, uma vez a albumina dentro da célula, o T3 se desprende da proteína para agir na mitocôndria, enquanto a albumina, agora descarregada do hormônio se difunde para fora do citoplasma.
Novamente uma explicação que dispensa a atividade da membrana celular para por para dentro a molécula de albumina. Evidências de que albumina e outras proteínas entram e saem da célula sem problema algum, sem gasto algum de energia, já existem de longa data [A][B].
AZIMOVA [1884] mostra claramente que o hormônio tireoidiano penetra no citoplasma da célula-alvo carreado por moléculas [A] e por difusão [B]; ou como argumentam, o hormônio tireoidiano “entra no citoplasma através da membrana externa e se localiza na membrana interna da mitocôndria e na sua matrix”.
E lembremos que o T3 é insolúvel em água, portanto jamais poderia se solubilizado no plasma. Ou no líquido intracelular. A verdade é que ele viaja todo o tempo associado a moléculas, especialmente proteínas.
A pré-albumina transtirretina, por exemplo, carreia o T3 para a mitocôndria, também para o núcleo.
Pensemos, por um instante, nas consequências de tais evidências.
Em primeiro lugar o óbvio: trata-se de uma fantasia – em todo caso muito lucrativa – a de fazer o paciente medir o hormônio “livre”, livre de proteínas ou outras moléculas carreadoras; as evidências são de que ele age carreado por elas e não “livre”. Tempo, sangue e dinheiro desperdiçados [J].
Segundo, temos a importância estratégica de se consumir proteínas suficientes na alimentação.
Sem elas, sem suficiente albumina, globulina e pré-albumina, poderemos desenvolver um tipo de hipotireoidismo particular: o hormônio ativo não terá como ser carreado. Ele existe, pode até ser suplementado, mas não será carreado para o local de ação [mitocôndria]. E todos os tecidos precisam receber T3, uns mais que outros, mas todos dependem das proteínas que devem trazer o seu T3.
Dito de outra forma, não será possível superar o hipotireoidismo, por mais que se suplemente com tireoide, se a pessoa apresenta um expressivo grau de desnutrição proteica.
Por exemplo, caso ela consuma proteína diariamente de forma minimalista, insuficiente. Não contará com aminoácidos para o corpo sintetizar as proteínas carreadoras. E o T3, que não se dissolve no plasma, precisa se associar a proteínas, a hemácias; na falta de proteínas, o T3 sequer desembarca da hemácia para entrar, novamente carreado, no citoplasma/mitocôndria.
Aliás, de passagem, vale a pena destacar o papel que o T3 vem ganhando na cirurgia cardiovascular.
Vem tornando os transplantes mais bem sucedidos, especialmente em cirurgia cardíaca [F]. Ao ponto de pesquisadores concluírem que “T3 possui um enorme impacto na redução da mortalidade cirúrgica e pode ser defendido como uma nova modalidade terapêutica em pacientes com mortalidade estimada alta quando passam por cirurgia de coração aberta” [G].
É importante em casos assim, saber qual o T3 medir, para que se possa dispor de uma avaliação séria da presença do T3 disponível. Isto é, tendo consciência de que o que se mede no plasma é uma mínima parte do que está no sangue e, ao mesmo tempo, valorizando muito mais a avaliação biológica da sua presença. E a necessidade de garantir suprimento proteico para aqueles pacientes antes da cirurgia.
Portanto, o caso da proteína é chave. Na verdade, ou algumas ideias do tipo clichê, são debatidas e reconsideradas na medicina, ou jamais entenderemos porque o consumo de proteína é tão crítico para se tratar o hipotireoidismo.
E quando se pretenda avaliar a função tireoidiana, para além da abordagem clínica [onde temperatura, pulso, pés frios e reflexo de Aquiles possuem sua notável importância], tem sua utilidade exames laboratoriais como TSH, T3 e T4, antiTPO, desde que interpretados – sempre interpretados - e não tomados pelo seu valor de face, como veremos em outra nota.
GM Fontes, Brasília, 4-5-23
As informações aqui presentes não pretendem servir para uso diagnóstico, prescrição médica, tratamento, prevenção ou mitigação de qualquer doença humana. Não pretendem substituir a consulta ao profissional médico ou servir como recomendação para qualquer plano de tratamento. Trata-se de informações com fins estritamente educativos.
Referências ____________________
[A] AZIMOVA ShS, UMAROVA, G D, 1984. [The nature of thyroid hormone receptors. Translocation of thyroid hormones through plasma membranes]. Biokhimiia . 1984 Aug;49(8):1350-6. [Article in Russian] PMID: 6093898 “The in vivo translocation of thyroxine-binding blood serum prealbumin (TBPA) was studied. It was found that the TBPA-hormone complex penetrates-through the plasma membrane into the cytoplasm of target cells. Electron microscopic autoradiography revealed that blood serum TBPA is localized in ribosomes of target cells as well as in mitochondria, lipid droplets and Golgi complex. Negligible amounts of the translocated TBPA is localized in lysosomes of the cells insensitive to thyroid hormones (spleen macrophages). Study of T4- and T3-binding proteins from rat liver cytoplasm demonstrated that one of them has the antigenic determinants common with those of TBPA. It was shown autoimmunoradiographically that the structure of TBPA is not altered during its translocation”.
[B] AZIMOVA ShS, UMAROVA G D, 1984. [The nature of thyroid hormone receptors. Thyroxine- and triiodothyronine-binding proteins of mitochondria]. Biokhimiia. 1984 Sep;49(9):1478-85. [Article in Russian] PMID: 6097306 “T4- and T3-binding proteins of rat liver were studied. It was found that the external mitochondrial membranes and matrix contain a protein whose electrophoretic mobility is similar to that of thyroxine-binding blood serum prealbumin (TBPA) and which binds either T4 or T3. This protein is precipitated by monospecific antibodies against TBPA.
The internal mitochondrial membrane has two proteins able to bind thyroid hormones, one of which is localized in the cathode part of the gel and binds only T3, while the second one capable of binding T4 rather than T3 and possessing the electrophoretic mobility similar to that of TBPA. Radioimmunoprecipitation with monospecific antibodies against TBPA revealed that this protein also the antigenic determinants common with those of TBPA. The in vivo translocation of 125I-TBPA into submitochondrial fractions was studied. The analysis of densitograms of submitochondrial protein fraction showed that both TBPA and hormones are localized in the same protein fractions. Electron microscopic autoradiography demonstrated that 125I-TBPA enters the cytoplasm through the external membrane and is localized on the internal mitochondrial membrane and matrix”.
[C] TERASAKI, T, PARDRIDGE, W M, 1987. Stereospecificity of Triiodothyronine Transport into Brain, Liver, and Salivary Gland: Role of Carrier- and Plasma Protein-Mediated Transport. Endocrinology, Volume 121, Issue 3, 1 September 1987, Pages 1185–1191, https://doi.org/10.1210/endo-121-3-1185 “The stereospecificity of T3 transport through the walls of the brain capillary, i.e. the blood-brain barrier (BBB), and the salivary gland capillary and through the hepatocyte plasma membrane was studied with a tissue-sampling single injection technique in rats. In the absence of plasma proteins, the ED50 of inhibition of the saturable transport of [125I]L-T3 through the BBB was 1 μM for unlabeled L-T3 and 9 ftM for unlabeled D-T3. The brain extraction of [125I]D-T3, 5.9 ± 0.1% (±SE), was about one third that of [125I]L-T3. Conversely, no saturable and no stereospecific T3 transport was observed for the salivary gland capillary, which, unlike the brain capillary, is porous. The hepatic extraction of T3 was minimally stereospecific in the absence of plasma proteins. In the presence of 5 g/dl bovine albumin, the fraction of circulating D- or L-T3 that was available for transport into liver (50-100%) was many-fold greater than the fraction that was free in vitro (-2%); therefore, both D-T3 and L-T3 were available for uptake by liver from the circulating albumin-bound pool.
This plasma protein-mediated transport of T3 is believed to represent a process of enhanced dissociation of T3 from the albumin-binding site, since the plasma protein per se is not significantly taken up by liver on a single pass. However, in the presence of 5 g/dl bovine albumin, the extravascular hepatic extraction of [125I]D-T3 (50 ± 2%) was nearly half that for [125I]T3 (93 ± 12%), although no significant difference in the in vitro binding of [125I]D-T3 and [126I]L-T3 to 5 g/dl bovine albumin was found with equilibrium dialysis. In addition, the isoelectric point of bovine albumin bound to [125I] L-T3 (5.1) was higher than that of bovine albumin bound to [125I] D-T3 (5.0), as determined by isoelectric focusing, which indicates that the surface of the bovine albumin molecule is slightly more positive when the protein binds L-T3 as opposed to D-T3. The isoelectric focusing and in vivo transport data together suggest that the interaction between the surfaces of the plasma protein and the hepatic microcirculation that is presumed to cause enhanced hormone dissociation from the protein-binding site is electrostatic in nature. These studies (1) show that the BBB thyroid hormone transport system is sharply stereospecific, and this property is probably a major factor underlying the low biological potency of D-T3 in brain; and (2) provide the first evidence for stereospecificity of plasma protein-mediated transport of hormones into tissues in vivo. (Endocrinology121:1185–1191,1987). https://academic.oup.com/endo/article-abstract/121/3/1185/2541424?redirectedFrom=fulltext
[D] MOORADIAN A D, 1990. Blood-brain transport of triiodothyronine is reduced in aged rats. Mech Ageing Dev . 1990 Mar 15;52(2-3):141-7. doi: 10.1016/0047-6374(90)90120-5. PMID: 2325430 DOI: 10.1016/0047-6374(90)90120-5. “An age-related decline in blood-brain barrier transport of thyroid hormones may contribute to the central nervous system changes with aging. To test this hypothesis, the brain uptake index (BUI) of levo (L) and dextro (D) triiodothyronine (T3) was determined in male Fischer 344 rats at 6 months of age (young) and 26 months of age (aged). Young rats pair fed with aged were included to control for reduced food intake in aged rats. The L-T3 BUI of aged rats (22.4 +/- 2.1%) was significantly reduced compared to young rats (29.5 +/- 2.0%) or young rats pair fed with aged rats (28.5 +/- 2.5%) (p less than 0.05). This could not be attributed to age-related changes in BBB permeability or to reduced cerebral blood flow. At steady state conditions, the brain uptake of either L-T3 or D-T3 was not altered with aging. There were no significant changes in plasma or brain binding of T3. These results indicate that the reduced BBB transport of T3 in aged rats is counterbalanced by a reduction in T3 clearance from the brain”.
[E] PARDRIDGE, W M, MIETUS L J, 1980. Transport of Thyroid and Steroid Hormones through the Blood-Brain Barrier of the Newborn Rabbit: Primary Role of Protein-Bound Hormone Endocrinology, Volume 107, Issue 6, 1 December 1980, Pages 1705–1710, https://doi.org/10.1210/endo-107-6-1705
The transport of [125I]T3 [125I]T4, [3H]testosterone, and [3H]estradiol through the blood-brain barrier (BBB) of the newborn rabbit was studied with a tissue-sampling, single injection technique. The first pass extractions of T3 and T4 were 22 ± 2% and 14 ± 1%, respectively, after carotid injection of Ringer's solution (0.025% albumin). Thyronine transport was saturated and cross-competitive, but was not inhibited by a large excess of leucine, a neutral amino acid. The extraction of T3 was reduced to 7 ± 1% after injection of hormone mixed in a 10% T3- specific rabbit antiserum, and this value approximated the extraction of an extracellular space marker, such as sucrose (6 ± 1%). Therefore, antibody-bound T3 was not available for transport in vivo. Conversely, T3 bound to the plasma proteins in newborn rabbit antiserum, e.g. albumin, was transported into the brain. The concentration of plasma protein required to inhibit T3 transport 50% in vivo was 28-fold greater than the serum concentration that resulted in 50% binding of T3in vitro.
The first pass extractions of testosterone and estradiol after injection of hormone in Ringer's solution were 100 ± 5% and 91 ± 5%, respectively. A 5 g/100 ml concentration of albumin bound about 95% of steroid in vitro, but resulted in only a 17–20% inhibition of testosterone or estradiol transport in vivo. Similarly, testosterone bound to the progesterone-binding globulin of pregnant guinea pig serum was also transported, although to a lesser extent than albumin-bound hormone. Conversely, testosterone bound to a specific rabbit antiserum, or testosterone or estradiol bound to the sex hormone-binding globulin in human serum was not transported into the brain. These results indicate that the mechanisms of thyroid and steroid hormone transport through the BBB of the newborn rabbit are very similar to those of the adult rat; therefore, the processes mediating BBB transport of protein-bound hormones are firmly established by at least the first 8–24 h of postnatal life. https://academic.oup.com/endo/article-abstract/107/6/1705/2591435?redirectedFrom=fulltext&login=false
[F] NOVITZKY D, 1996. Novel actions of thyroid hormone: the role of triiodothyronine in cardiac transplantation. Thyroid . 1996 Oct;6(5):531-6. doi: 10.1089/thy.1996.6.531. PMID: 8936684 DOI: 10.1089/thy.1996.6.531 “In clinical heart transplantation, the heart is procured from brain dead (BD) organ donors who acutely experienced a variety of critical illnesses. In all of these conditions, a profound derangement of the thyroid profile has been observed. Although the plasma levels of thyroid stimulating hormone (TSH) remain unchanged, there is a rapid decline in free triiodothyronine (FT3) levels (p < 0.0001) as well as an elevation of reverse triiodothyronine (rT3) (p < 0.001). Following induction of experimental brain death, the heart exhibits a progressive significant hemodynamic-biochemical deterioration (reduction of cardiac contractility, depletion of high energy phosphates, glycogen, and accumulation of tissue lactate). The administration of T3 to BD animals resulted in rapid reversal of the hemodynamic and metabolic derangements.
The impact of T3 therapy to unstable human brain dead organ donors has resulted in rapid hemodynamic stability allowing significant reduction of inotropic support (p < 0.001). These hearts, following cardiac transplantation, exhibited excellent hemodynamic function in the recipients. The low FT3 state has also been observed during and following open heart surgery on cardiopulmonary bypass (CPB). Therefore, at the completion of the heart transplant procedure, T3 was also administered to the recipient to prevent relapse of the hemodynamic-metabolic abnormality observed in the donor. The impact of T3 therapy to initially unstable donors allowed for rapid inotropic reduction and recovery of the heart, thus enlarging the donor organ pool and improving the outcome of the recipients following cardiac transplantation”.
[G] NOVITZKY D, FONTANET H, 1996. Impact of triiodothyronine on the survival of high-risk patients undergoing open heart surgery. Cardiology . 1996 Nov-Dec;87(6):509-15. “Experimental and clinical studies have shown the beneficial effects of triiodothyronine (T3) following myocardial revascularization on cardiopulmonary bypass (CPB). In this study, open-label T3 was administered to 68 high-risk patients undergoing open heart surgery. The New Jersey Risk Assessment was used to calculate the preoperative estimated surgical mortality. A loading dose of T3 was administered: (a) at release of the aortic cross-clamp, (b) whenever the patient became CPB dependent, (c) if the patient exhibited low cardiac output after discontinuing CPB and (d) as pretreatment before initiating CPB. All therapeutic modalities were followed by a continuous T3 infusion. Following T3 therapy, CPB was discontinued in all patients. Based upon discriminant analysis, a total of 26 deaths were expected from the entire group, but only 7 patients died, therefore, the observed mortality was reduced by 72% (p < 0.007). The use of T3 had a major impact on reducing surgical mortality, and may be advocated as a new therapeutic modality in patients with high estimated mortality undergoing open heart surgery”. Disponível em: https://pubmed.ncbi.nlm.nih.gov/8904679/
[H] MOREAU X, LEJEUNE P J, 1999. Kinetics of red blood cell T3 uptake in hypothyroidism with or without hormonal replacement, in the rat. J Endocrinol Invest . 1999 Apr;22(4):257-61. doi: 10.1007/BF03343553. PMID: 10342358 DOI: 10.1007/BF03343553 “L-triiodothyronine (L-T3) is taken up and accumulated into red blood cells (RBC) by means of a specific carrier-mediated system. The aim of this study was to evaluate the reactivity of this system in relation to induced alterations in thyroid hormone (TH) supply. We investigated the kinetic parameters (Vmax, maximal velocity and Km, Michaelis constant) of washed-RBC L-T3 uptake 1) in thyroidectomized (TXT) rats, 2) in TXT rats administered with low doses of L-T4 (15 microg/kg/day x 14) to restore normal serum TH levels (REPL), 3) in TXT rats administered with high doses of L-T4 (200 microg/kg/day x 14) to achieve a large increase in serum TH levels (HIGH).
Serum free T3 and T4 levels were significantly decreased in TXT rats (2.4 and 8.8 fold, respectively), not different in REPL rats and significantly increased in HIGH rats (2.4 and 3 fold, respectively) compared to sham-operated rats (SHAM). Both kinetics of RBC L-T3 uptake were significantly increased in TXT rats (Vmax+/-SE in pmol/min/10(8) cells=235.1+/-11.1, p<0.05 and Km+/-SE in nM=190.1+/-9.0, p<0.05), not different in REPL rats (Vmax=1 84.8+/-7.6 and Km=151.9+/-7.1) and significantly decreased in HIGH rats (Vmax=168.0+/-4.1, p<0.01 and Km=131.9+/-4.6, p<0.01) compared to SHAM rats (Vmax=197.7+/-5.8 and Km=160.9+/-6.1). These results show that kinetics of RBC L-T3 uptake are modified in response to defect or excess in circulating TH levels. Since RBC play likely a role of a buffer system, the changes in carrier-mediated influx of L-T3 could be seen as a compensatory mechanism that counteract the disturbances in the TH availability for the target tissues”.
[J] Conversando com um professor, médico que dá aulas sobre exames laboratoriais, no Rio de Janeiro, anos atrás, lembro que ele defendeu que o mais moderno é usar apenas T3 e T4 “livres”. Ele se considerava atualizado. Mostra como caminha a medicina. Não custa lembrar, em todo caso, que se trata do mesmo profissional que defende reposição de estrogênio e também que colesterol deveria ser sempre menor que 170 [mesmo que tivesse que se usar estatinas] para se ter uma boa saúde, defendendo, portanto, o clichê do colesterol vilão cardiovascular. Um poço de contradições. Mas não se deu ao trabalho de dar alguma explicação sobre como o T3, por exemplo, poderia ser “livre” se não se dissolve em água [plasma] e se toda a tatividade tireoidiana pode ser explicada pelo efeito biológico, sem se ter que recorrer o conceito do hormônio “livre”.
[L] McLEESE, J M, EALES J G, 1996. Characteristics of the uptake of 3,5,3'-triiodo-L-thyronine and L-thyroxine into red blood cells of rainbow trout (Oncorhynchus mykiss). Gen Comp Endocrinol. 1996 Aug;103(2):200-8. doi: 10.1006/gcen.1996.0111. PMID: 8812373 DOI: 10.1006/gcen.1996.0111 “The mechanisms of uptake of thyroid hormones (TH) 3,5,3'-triiodo-L-thyronine (T3) and L-thyroxine (T4) by trout red blood cells (RBC) were characterized by coincubating washed RBC with [125I]T3 or [125I]T4 and a variety of inhibitors and potentially competing amino acids and TH analogues. Nonsaturable uptake of both TH was unaffected by almost all agents tested, consistent with a diffusion process. Saturable T3 uptake was unaffected by a major (80%) cyanide- and iodoacetate-induced reduction in RBC nucleotide triphosphate content or by inhibitors of Na+ transport, but was depressed by (i) inhibitors of protein binding (bromosulfophthalein, 8-anilino-1-naphthalene sulfonic acid, phloretin, and 5,5'-diphenylhydantoin, (ii) sulfhydryl blockers (p-hydroxy-mercuribenzoate and N-ethylmaleimide), (iii) endocytotic inhibitors (chloroquine, colchicine, and monodansylcadaverine), (iv) tryptophan and phenylalanine, and (v) certain TH analogues, particularly 3,3',5'-triiodo-L-thyronine (reverse T3). In contrast, saturable T4 uptake was depressed only by inhibitors or protein binding. Cross-competition between T3 and T4 for transport occurred only at highly pharmacologic TH levels. We conclude that T3 and T4 are transported into trout RBC by two separate systems. The relatively slow T4 uptake depends on binding to certain proteins. The much more rapid T3 uptake depends on protein binding, but is Na(+)-independent, and involves a system comparable to the T-system of aromatic amino acid transport. However, participation od receptor-mediated endocytosis cannot be excluded”.
GOUMAZ, M O, KAISER C , 1987. Brain cortex reverse triiodothyronine (rT3) and triiodothyronine concentrations under steady state infusions of thyroxine and rT3. Endocrinology. 1987 Apr;120(4):1590-6. doi: 10.1210/endo-120-4-1590. PMID: 3830062 DOI: 10.1210/endo-120-4-1590 “T4 and reverse T3 (rT3) can inhibit 5'-deiodinase type II activity in rat brain cortex, pituitary, and brown adipose tissue, raising the possibility that T4 may act in vivo after conversion to rT3. The aim of this study was to measure in hypothyroid (Tx) rats the content of brain cortex rT3 during a constant 7-day infusion of either [125I]T4 alone, corresponding to 12 pmol T4/day X 100 g body weight (BW), or together with 400 pmol T4/day. [125I]T4, rT3, and T3 were extracted from brain cortex, pituitary, kidney, and liver with a combination of adsorption chromatography on Sephadex G-25, HPLC, and immunoprecipitation. [131I]T4, T3, or rT3 were used as internal standards. [125I]rT3 could be detected in brain cortex, liver, and kidney in Tx rats infused with [125I]T4 (12 pmol T4/day X 100 g BW) and in those infused with 400 pmol T4/day X 100 g BW. The highest rT3 concentrations were found in brain cortex, where it represented 6% to 10.5% of the local T4 concentration.
During an infusion of 400 pmol T4/day X 100 g BW, brain cortex T3 concentration was 6 times higher in the brain cortex than in serum, and even exceeded that of T4. In Tx rats receiving [125I]T4 alone the brain cortex to serum T3 ratio was 3:1, but the total serum T3 concentration, measured by RIA, was much higher than that due to conversion [0.50 +/- (SE) 0.1 pmol/ml vs. 0.018 +/- 0.002 pmol T3/ml], indicating thyroidal secretion. The effect of the blood-brain barrier on rT3 was measured by infusing [125I]rT3 over 4 days. After killing, rT3 was isolated as above. Approximately 3% of serum rT3 was retrieved from the brain cortex, whereas during the T4 infusion 40-50% of serum rT3 was found demonstrating that brain cortex rT3 is locally produced”.
[N] PARDIDGE, W M LANDAW E M, 1984. Tracer kinetic model of blood-brain barrier transport of plasma protein-bound ligands. Empiric testing of the free hormone hypothesis. J Clin Invest . 1984 Sep;74(3):745-52. doi: 10.1172/JCI111490. PMID: 6470138 PMCID: PMC425228 DOI: 10.1172/JCI111490 “Pevious studies have shown that the fraction of hormone or drug that is plasma protein bound is readily available for transport through the brain endothelial wall, i.e., the blood-brain barrier (BBB). To test whether these observations are reconcilable with the free-hormone hypothesis, a tracer-kinetic model is used in the present investigations to analyze in vivo initial extraction data on BBB transport of protein-bound steroid hormones (dihydrotestosterone, testosterone, estradiol, and corticosterone), thyroid hormones (triiodothyronine), and lipophilic amine drugs (propranolol).
The plasma proteins used are bovine albumin and human orosomucoid. Transport data was fit to a modification of the Kety-Renkin-Crone equation of capillary physiology; the modified equation incorporates the principles of both capillary physiology and plasma protein-ligand mass action binding relationships. In most cases, the experimental data is best fit to the model equation when the apparent in vivo dissociation constant, KDa, of the ligand protein binding reaction increases to values that are 5- to 50-fold greater than the in vitro dissociation constant, KD. This result indicates that the rate of ligand dissociation from the plasma protein is accelerated in the capillary bed relative to the in vitro situation. It is hypothesized that the major factor leading to the rapid transport in vivo of protein-bound ligands into tissues such as brain is an endothelial-induced decrease in the affinity of the plasma protein for the ligand. Under these conditions, the amount of plasma ligand available for tissue clearance in vivo parallels the protein-bound fraction, not the free hormone”.
[O] DRATMAN, M B, CRUTCHFIELD, F L, 1991. Transport of iodothyronines from bloodstream to brain: contributions by blood:brain and choroid plexus:cerebrospinal fluid barriers. Brain Res . 1991 Jul 19;554(1-2):229-36. doi: 10.1016/0006-8993(91)90194-z. PMID: 1933305 DOI: 10.1016/0006-8993(91)90194-z “Thyroid hormone entering the brain from the cerebral circulation must first cross barriers at the the blood:brain and choroid plexus:cerebrospinal fluid interfaces. The route taken after entry through those barriers might bring about selective delivery of hormone to different regions of the brain and those differences might be crucial for the ultimate functional effects of the hormone. To determine whether and how distribution of hormone in the brain might vary according to the route of entry, film autoradiograms of serially sectioned brains were prepared after delivery of a pulse of 125I-labeled thyroid hormone into either the right lateral cerebral ventricle or the femoral vein. The results after intrathecal injection, reflecting the penetration of hormone into brain after crossing the choroid plexus:cerebrospinal fluid barrier, revealed a markedly limited, essentially periventricular distribution of radioactivity at both 3 and 48 h after hormone administration.
Results after i.v. administration, which allows hormone access across both barriers, revealed an initial distribution pattern (at 3 h) generally similar to that seen after administration of markers of cerebral blood flow; at 48 h there was strong resolution in selected brain regions never noted to be labeled after intrathecal hormone injection. The functional implications of the differences in results produced by the two different routes of hormone entry are not known. However, ready access to circumventricular organs would appear to be favored by hormone crossing the choroid plexus:cerebrospinal fluid barrier whereas access to the panoply of nuclear triiodothyronine receptors would be favored by hormone crossing the blood:brain barrier. Therefore both routes of barrier transport should be taken into account in assessing the kinetics and actions of thyroid hormones in the central nervous system”.
[P] KOIBUCHI N MATSUZAKI S, 1996. Ontogenic changes in the expression of cytochrome c oxidase subunit I gene in the cerebellar cortex of the perinatal hypothyroid rat. Endocrinology . 1996 Nov;137(11):5096-108. doi: 10.1210/endo.137.11.8895384. PMID: 8895384 DOI: 10.1210/endo.137.11.8895384 “The thyroid hormone plays a critical role in normal development of the mammalian central nervous system. This study was designed to examine the effect of perinatal hypothyroidism on ontogenic change in cytochrome c oxidase subunit I (COX I) gene expression in the rat cerebellum by using quantitative in situ hybridization histochemistry (ISH). Newborn rats were rendered hypothyroid by continuous administration of methimazole in the mothers' drinking water. The pups were then killed by decapitation on 1, 5, 10, 15, 20, and 30 days after birth (P1, P5, P10, P15, P20, and P30). Their cerebella were removed, and frozen sections were cut and processed for ISH with 35S-labeled RNA probe for COX I messenger RNA. After hybridization, emulsion autoradiography was performed. The numbers of grains within the external granule cell layer, molecular layer, and internal granule cell layer were then counted. A significant decrease in grain density was detected in the hypothyroid animal in all these areas on P5, P10, and P15. On P15, in the molecular layer, a greater hybridization signal was detected in the inner portion than in the outer portion in the euthyroid animal.
No such difference was seen in the hypothyroid animal. Daily T4 treatment for 15 days restored the effect of methimazole treatment. The significant effect of perinatal hypothyroidism on COX I gene expression was not detected after P20. These results indicate that altered thyroid states affect the COX I gene expression in the cerebellar cortex during development, suggesting that the COX I gene is one of the key genes regulated by the thyroid hormone and plays an important role in the morphogenetic changes observed in the perinatal hypothyroid cerebellum”.
[Q] LUXON, B A, MILLIANO M T, 1997. Cytoplasmic codiffusion of fatty acids is not specific for fatty acid binding protein. Am J Physiol . 1997 Sep;273(3 Pt 1):C859-67. doi: 10.1152/ajpcell.1997.273.3.C859. PMID: 9316406 DOI: 10.1152/ajpcell.1997.273.3.C859 “The intracellular movement of fatty acids is thought to be facilitated through codiffusion with fatty acid binding protein (FABP). Previous work suggested that FABP decreases fatty acid binding to immobile membranes, causing faster cytoplasmic diffusion. However, the specificity for binding to FABP has not been addressed. The aim of the current study was to determine whether specific FABP binding is required or whether binding to other proteins will produce the same effect. A model cytoplasm consisted of a fatty acid, proteins, and liposomes to simulate intracellular membranes.
Laser photobleaching (fluorescence recovery after photobleaching) was used to measure the movement of the fluorescent fatty acid 12-N-methyl-7-nitrobenzo-2-oxa-1,3-diazoaminostearate (NBD-stearate) in model cytoplasm, in normal and permeabilized Hep G2 cells, and after incubation of permeabilized cells with bovine serum albumin (BSA) or FABP. Increasing protein in the model cytoplasm increased the diffusion rate in proportion to the extent of protein binding. Cell permeabilization reduced diffusion of NBD-stearate to < 5% of controls. Incubation of permeabilized cells with FABP or BSA resulted in a concentration-dependent increase in the NBD-stearate diffusion rate. BSA was more effective than FABP in binding NBD-stearate and increasing its diffusion rate after permeabilization. Proteins like FABP promote the diffusion of fatty acids. Removal of these proteins drastically reduces cytoplasmic diffusion. Substitution with BSA reestablishes the diffusive flux, suggesting that specific binding to FABP is not required. These data support a role for intracellular binding proteins in facilitating the cytoplasmic movement of fatty acids”.
[R] MOREAU X, AZORIN J M, 1998. Increase in red blood cell triiodothyronine uptake in untreated unipolar major depressed patients compared to healthy volunteers. Prog Neuropsychopharmacol Biol Psychiatry . 1998 Feb;22(2):293-310. doi: 10.1016/s0278-5846(98)00005-0. PMID: 9608602 DOI: 10.1016/s0278-5846(98)00005-0 “1. Kinetic parameters of red blood cell (RBC) L-triiodothyronine (T3) initial uptake (Vmax, maximal velocity and Km, Michaelis constant) were determined in 34 untreated inpatients suffering from unipolar depression and in 40 healthy volunteers. 2. Both Vmax and Km were significantly increased in depressed patients as compared to controls. The alterations in kinetic parameters were not associated with the severity of depression. 3. Out of the 19 depressed patients who were submitted to TRH test, 7 of them (36%) showed a blunted TRH-induced TSH response associated with a Vmax situated outside the control mean value +/- 1 S.D. 4.
The authors found a significant positive correlation between Vmax of RBC L-T3 and L-tryptophan (TRP) uptakes which is in agreement with the assumption that L-T3 and L-TRP share a common carrier system at the erythrocyte level. 5. The results indicate that the uptake of L-T3 by RBC is increased in major depression. These transport perturbations might reflect alterations in the plasmatic metabolism of L-T3. Evaluation of RBC L-T3 uptake could be useful in a best biological characterization of the depressed patients with regard to their thyroid function”.
[S] DOCTER, R, KRENNING E P, 1982. Evidence that the uptake of tri-iodo-l-thyronine by human erythrocytes is carrier-mediated but not energy-dependent. Biochem J. 1982 Oct 15; 208(1): 27–34. doi: 10.1042/bj2080027 PMCID: PMC1153924 PMID: 7159396 “We investigated 3,3′,5-tri-iodo-l-thyronine transport by human erythrocytes and by `ghosts' prepared from these cells. Uptake of tri-iodothyronine by erythrocytes at 37°C was time-dependent with a maximum reached after 60min. Tracer analysis after incubation for 1min revealed only one saturable binding site, with Km 128±19nm (mean±s.e.m.; n=7) and Vmax. 4.6±0.7pmol of tri-iodothyronine/min per 6×107 cells. After 10min incubation Km 100±16nm (n=10) was found with Vmax. 7.7±1.2pmol of tri-iodothyronine/10min per 6×107 cells. At 0°C the uptake system is still active, with Km 132±26nm and Vmax. 1.8±0.3pmol of tri-iodothyronine/10min per 6×107 cells. The Vmax. with intact cells is 5-fold greater than the Vmax. with membranes derived from the same amount of cells when uptake studies are performed in media with similar free tri-iodothyronine concentrations. This indicates that at least 80% of tri-iodothyronine taken up by the intact erythrocytes enters the cell.
This saturable uptake system can be inhibited by X-ray-contrast agents in a dose-dependent fashion. (±)-Propranolol, but not atenolol, has the same effect, indicating that the membrane-stabilizing properties of (±)-propranolol are involved. Furthermore, there is no inhibition by ouabain or vanadate, which indicates that tri-iodothyronine uptake is not dependent on the activity of Na++K+-dependent adenosine triphosphatase. We have prepared erythrocyte `ghosts', resealed after 2.5min with 0mm-, 2mm- or 4mm-ATP inside. Inclusion of ATP and integrity of the membrane of the erythrocyte `ghosts' were verified on the basis of an ATP-concentration-dependent functioning of the Ca2+ pump. No difference was found in the uptake of tri-iodothyronine by erythrocyte `ghosts' with or without ATP included, indicating that uptake of tri-iodothyronine is not ATP-dependent. The following conclusions are drawn. (1) Tri-iodothyronine enters human erythrocytes. (2) There is only one saturable uptake system present for tri-iodothyronine, which is neither energy (i.e. ATP)-dependent nor influenced by the absence of an Na+ gradient across the plasma membrane. This mode of uptake of tri-iodothyronine by human erythrocytes is in sharp contrast with that of rat hepatocytes, which uptake system is energy-dependent and ouabain-sensitive [Krenning, Docter, Bernard, Visser & Hennemann (1978) FEBS Lett. 91, 113–116; Krenning, Docter, Bernard, Visser & Hennemann (1980) FEBS Lett. 119, 279–282]. (3) X-ray-contrast agents inhibit tri-iodothyronine uptake by erythrocytes in a similar fashion to that by which they inhibit the uptake of tri-iodothyronine by rat hepatocytes [Krenning, Docter, Bernard, Visser & Hennemann (1982) FEBS Lett. 140, 229–233]”. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1153924/
[T] OSTY J VALENSI P, 1990. Transport of thyroid hormones by human erythrocytes: kinetic characterization in adults and newborns. J Clin Endocrinol Metabolismo . 1990 Dec;71(6):1589-95. doi: 10.1210/jcem-71-6-1589. PMID: 2229315 DOI: 10.1210/jcem-71-6-1589 “The uptake of [125I]T3 and [125I]T4 by human erythrocytes was studied. The erythrocytes were obtained from adult subjects (28-41 yr old) and suspended in a protein-free medium. The half-times of equilibration for both T3 and T4 were 6 min. At equilibrium, T3 was concentrated 55-fold inside the cells, while T4 was concentrated 40 times, but these accumulations were not dependent on either cellular ATP or the transmembrane Na+ gradient. The amounts of cell-associated thyroid hormones were 20 times (T3) and 17 times (T4) higher than the amounts of free extracellular hormones at 5 X 10(9) erythrocytes/mL (the blood concentration). Oligomycin and phloretin inhibited T3-saturable transport (but not T4 transport) independently of cellular energy. We suggest that thyroid hormones are concentrated by intracellular trapping.
The rates of T3 and T4 efflux from preloaded erythrocytes were similar to the influx rates. The initial velocities of T3 (but not T4) uptake and efflux were 70% saturable. The uptake was specific because the unlabeled analogs T4, triiodothyroacetic acid, rT3, D-T3, and D,L-thyronine inhibited [125I]T3 uptake 60, 125, 160, 190, and 1600 times less, respectively, than did unlabeled T3. The kinetic parameters of T3-saturable uptake, Km, and maximum velocity were determined for three groups of subjects: newborns, 28 to 41-yr-old adults, and 76 to 90-yr-old adults. The Km (67 nmol/L in 28 to 41-yr-old adults) was not age dependent, BUT the maximum velocity was significantly higher in newborns than in adults. We conclude that T3 transport across the human erythrocyte membrane is mediated mainly by facilitated diffusion, whereas T4 transport results from free diffusion. Human erythrocytes might act as a circulating pool of thyroid hormones, especially T3 in newborns”.
[U] A bibliografia acima foi sugerida por R. Peat, no seu texto Thyroid, therapy, confusion and fraud, de 2014.
***